Epilepsy and anti-epileptics
- 22 Dec 2023
- 3 Minutes to read
- Print
- PDF
Epilepsy and anti-epileptics
- Updated on 22 Dec 2023
- 3 Minutes to read
- Print
- PDF
Article summary
Did you find this summary helpful?
Thank you for your feedback
This section covers:
- Epilepsy and the menopause transition
- Epilepsy and HRT
- Use of Lamotrigine
- Use of Liver enzyme inducers
- Other anti-epileptic medications
1. EPILEPSY AND THE MENOPAUSE TRANSITION
- Oestrogen and progesterone can affect neuronal excitability.
- Around 40% of women have more seizures at certain times in their monthly cycle. This is called 'catamenial epilepsy'.
- Seizure risk may increase in some women during the menopause transition, however for others it may decrease, and for many there will be no change in risk.
- Women with catamenial epilepsy often have more seizures during perimenopause with gradual improvement over time as they reach the postmenopause phase.
- Women should be advised to maintain a healthy lifestyle with regular exercise and a balanced diet. Triggers that provoke seizures should be minimised, such as stress, fatigue, drinking excessive alcohol and poor sleep.
- Women with frequent seizures reach menopause 3-5 years earlier than average.
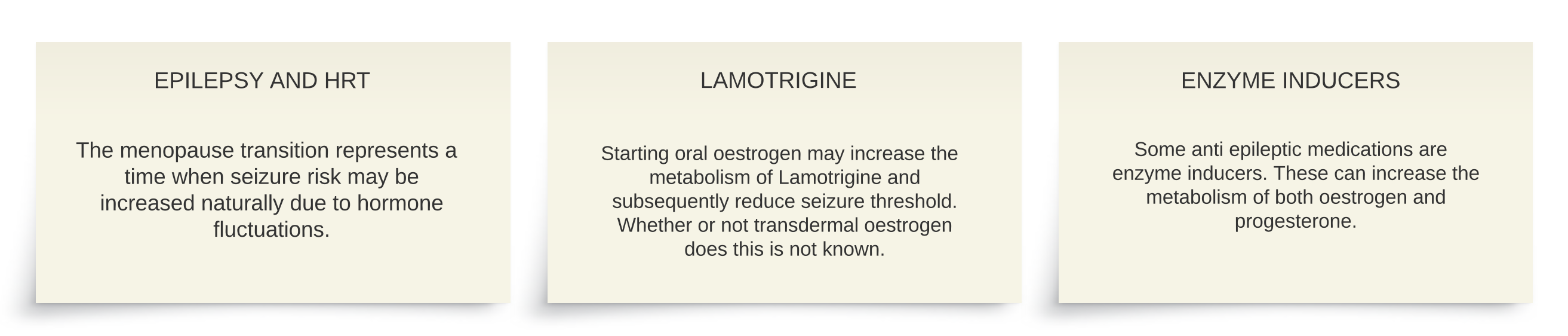
2. EPILEPSY AND HRT
- Women with epilepsy can take HRT and epilepsy is not a reason to avoid HRT.
- Uncontrolled menopausal symptoms such as night sweats and poor sleep may increase seizure risk in some women.
- Data about epilepsy and HRT however is limited.
- The only information from clinical trials was with older types of HRT that used oral combined preparations containing conjugated equine estrogens. This older type of HRT increased seizure frequency.
- Whether the increase in seizure frequency is the effect of the oestrogen, or the effect of the progestogen, is unclear due to a lack of research. Although in general, oestrogen is considered to increase the risk of seizures and progesterone lower it.
- It is likely that newer types of HRT that use transdermal estradiol have less effect on seizures, although more research is needed to confirm this.
- If HRT is prescribed a transdermal oestrogen should be used, starting at a low dose. This gives steadier levels of oestrogen in the body. Where a progestogen is needed, body identical progesterone might have specific benefits for epilepsy by increasing the effects of the brain chemical GABA.
- Women should be made aware of the above information and it would be good practice to update the patient’s neurologist. Where HRT is initiated or adjusted, epilepsy should be monitored.
2. USE OF LAMOTRIGINE
- Oral oestrogens can increase the metabolism of Lamotrigine and reduce its effectiveness.
- Starting oral oestrogen might reduce seizure threshold in a woman using Lamotrigine for epilepsy.
- Whether or not transdermal HRT does this is not known.
- Robust data is lacking, and so a cautious approach is recommended in women using Lamotrigine and advice should be sought from the patient’s neurology team.
- Sometimes, following neurology input, Lamotrigine levels are checked or the dose of Lamotrigine increased, however there is not a consensus view on this management.
3. USE OF LIVER ENZYME INDUCERS
- Some anti-epileptic medications are liver enzyme inducers.
- Examples of liver enzyme inducers include carbamazepine, eslicarbazepine, cenobamate, fosphenytoin, oxcarbazepine, perampanel, phenobarbital, primidone, phenytoin, fufinamide and topiramate.
- Liver enzyme inducers can increase the metabolism of oestrogens and progestogens, making the level of these hormones less effective compared to using usual doses.
- These women may need a slightly higher dose of HRT to relieve symptoms. In addition, there should be consideration to using a higher dose of a progestogen to ensure adequate endometrial protection.
4. OTHERS
- Anti-epileptic medications that do not significantly affect or interact with HRT include brivacetam, clonazepam, ethosuximide, fenfluramine, gabapentin, lacosamide, levetiracetam, piracetam, pregabalin, sodium valproate, tiagabine, stiripentol, vigabatrin, zonisamide.
- This list is not exhaustive.
Further Information:
- MacGregor A. Epilepsy, the menopause and HRT. Women's Health Concern Factsheet. Dec 2023.
- Briggs P. A brief review of women reporting seizures. Post Reprod Health. 2019.
- Erel C, Brincat M, Gambacciani M et al. EMAS position statement: managing the menopause in women with epilepsy. Maturitas. 2010.
- Baber R, Panay N, Fenton A. 2016 IMS recommendations on women’s midlife health and menopause hormone therapy. Climacteric. 2016. Found on page 125.
- Hillard T, Abenethy K, Hamoda H et al. BMS handbook. Management of the Menopause Sixth edition. British Menopause Society. 2017.
- Harden CL, Herzog AG, Nikolov BG, et al. Hormone replacement therapy in women with epilepsy: a randomized, double-blind, placebo-controlled study. Epilepsia 2006.
- Hamoda H. Progestogens and endometrial protection. British Menopause Society. Tools for clinicians. 2021. Found on page 5.
- Hormone replacement with estrogens may reduce lamotrigine serum concentrations: a matched case-control study. Epilepsia (Copenhagen). 2017.
Was this article helpful?

